ACL Tear & Reconstruction - Knee Ligament Injury
Introduction
The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments in the knee. Ligaments are strong non-elastic fibers that connect our bones together. The ACL crosses inside of the knee, connecting the thighbone to the leg. It provides stability to the knee joint.
ACL tears most commonly occur in very active people or athletes. The ACL can tear when people abruptly slow down from running, land from a jump, or change directions rapidly. These types of actions are frequently performed during sports, such as football, basketball, skiing, and soccer. Athletes are especially at risk for ACL tears, although they may occur in active workers and the general population as well.
The ACL can tear completely or partially. It is unable to repair itself. When the ACL is injured, it is common to see other surrounding knee structures damaged as well. Some cases of ACL tears are treated with non-surgical methods. However, there are several surgical options that successfully restore knee strength and stability.
Causes
The ACL can tear during strong twisting motions of the knee. The ACL can also tear if the knee is hyperextended or bent backwards. People frequently tear the ACL while pivoting, landing awkwardly from a jump, changing directions suddenly, or abruptly slowing down from running. ACL tears occur most frequently in young athletes. Football, basketball, skiing, and soccer are sports associated with the highest injury rates.
Researchers show that female athletes have a higher rate of ACL injury than males in certain sports. They suspect the greater angles in the female hip and leg alignment may make the knee more vulnerable to force. Additionally, female hormones can relax ligaments and make them less stable, making some women more susceptible to knee injury.
ACL tears occur most frequently in young athletes. Football, basketball, skiing, and soccer are sports associated with the highest injury rates.
Symptoms
People usually experience pain, swelling, and knee instability immediately after the ACL tears. Your knee may buckle or give out on you. You may not be able to fully straighten your knee. You may have difficulty moving your knee and walking. Typically, within a few hours the swelling in the knee increases dramatically.
Diagnosis
If you suspect you have torn your ACL, you should go to your doctor or an emergency room right away. A doctor can evaluate your knee by gathering your medical history, performing a physical examination, and viewing medical images. Your doctor will ask you about your symptoms and what happened if you were injured. Your doctor will examine your knee and your leg alignment. You will be asked to perform simple movements to help your doctor assess your muscle strength, joint motion, and stability.
Your physician will order X-rays to see the condition of the bones in your knee and to identify fractures. Sometimes a fracture or soft tissue injury does not show up on an X-ray. In this case, your doctor may order a magnetic resonance imaging (MRI) scan. An MRI scan will provide a very detailed view of your knee structure. Like the X-ray, the MRI does not hurt and you need to remain very still while the images are taken.
Treatment
Initially following an injury, your knee will be treated with rest, ice, compression, and elevation. You should rest your knee by not placing weight on it. You may use crutches to help you walk. Applying ice packs to your knee can help reduce pain and swelling. You should apply ice immediately after injuring your knee. Your doctor will provide you with a continued icing schedule. Your doctor may provide over-the-counter or prescription pain medication. In some cases, a knee brace may be recommended to immobilize and support the knee. A knee immobilizer is used for only a short period of time. Elevating your knee at a level above your heart helps to reduce swelling.
Physical therapy and rehabilitation can help restore knee functioning for some individuals. Your physical therapist will help you strengthen your knee. Special emphasis is placed on exercising the quadriceps muscles on the front of the thigh and the hamstring muscles on the back of the thigh. Eventually, you will learn exercises to improve your balance and coordination. You may need to wear a knee brace during activities. Your therapists will educate you on how to prevent further injury.
Surgery
Surgical treatment is most frequently recommended for individuals with ACL tears accompanied with other injuries. The most likely candidates for surgical treatment are active individuals in sports or jobs with heavy manual work that requires pivoting or pushing off with the knee. Surgery is also recommended for people with unstable knees or injuries combined with damage to the menisci, articular cartilage, joint capsule, or ligaments.
The goal of ACL repair is to reconstruct your knee joint to restore its function and stability, and prevent further injury. During surgery, your doctor will replace your damaged ACL with a healthy tendon, called a graft. There are several options for acquiring grafts. They may be taken from an area near your knee or from a donor cadaver.
Recovery
You will most likely go home on the same day of your surgery. You will receive pain medication to make you feel as comfortable as possible. In some cases, ice is applied to the knee throughout the day to help to reduce pain and swelling. Your doctor may prescribe blood thinning medication and special support stockings. You should keep your leg elevated and move or pump your foot and ankle.
Prevention
It is important that you adhere to your exercise program and safety precautions when you return home. You should stay as active as possible. It is especially important to keep your quadriceps and hamstrings very strong. You should also continue to use the durable medical equipment as advised.
It is also important to avoid injuring your ACL again. Depending on your injury, your surgeon may provide you with temporary or permanent activity or lifting restrictions. In some cases, specialized knee braces may be recommended for specific activities.
Ankle Sprain & Instability
Introduction
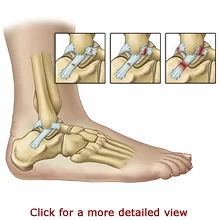
Ankle Sprains are a very common injury that can happen to anyone. Our ankles support our entire body weight and are vulnerable to instability. Walking on an uneven surface or wearing the wrong shoes can cause a sudden loss of balance that makes the ankle twist. If the ankle turns far enough, the ligaments that hold the bones together can overstretch or tear, resulting in a sprain. A major sprain or several minor sprains can lead to permanent ankle instability.
Causes
Our ankles are susceptible to instability, especially when walking on uneven surfaces, stepping down at an angle, playing sports, or when wearing certain shoes, such as high heels. Everyone, even the fittest athlete, is vulnerable to a sudden loss of balance under these conditions. Our ankles support our entire body weight. When the foot is placed at an abnormal angle, the weight of our body places an abnormal amount of force on the ligaments causing them to stretch. When a ligament is forced to stretch beyond its limit, it may overstretch, tear, or disconnect from the bone.
Symptoms
You may lose your balance and fall if your foot is placed at a poor angle on the ground. Some individuals may hear a “pop” noise when the injury takes place. You will probably have difficulty putting weight on your foot or walking. Pain is usually the first symptom of a Sprained Ankle. Swelling, stiffness, and skin discoloration from bruising may occur right away or take a few hours to develop.
Diagnosis
Your doctor can diagnose a Sprained Ankle by conducting a physical examination and asking you what happened to cause the injury. Your doctor will move your ankle in various positions to determine which ligament was injured. Your ankle may be X-rayed to make sure that you do not have a broken bone in your ankle or foot. In severe cases, a Magnetic Resonance Imaging (MRI) scan may be ordered to view the ankle structures in more detail. The X-ray and the MRI scan are painless and require that you remain very still while the images are taken.
Treatment
The majority of Ankle Sprains heal with non-surgical treatment methods. It is imperative that you seek evaluation and treatment for any ankle injury, as sometimes fractures are mistaken for sprains.
The treatment of an Ankle Sprain depends on its Grade. Grade One sprains are treated with the RICE method - Rest, Ice, Compression, and Elevation. You should rest your ankle by not placing weight on it. You may use crutches to help you walk. Applying ice packs to your ankle can help keep the swelling down and reduce pain. You should apply ice immediately after spraining your ankle. Your doctor will provide you with a continued icing schedule. Your doctor may recommend over-the-counter or prescription pain medication. Compression bandages, such as elastic wraps, are helpful to immobilize and support the ankle. You should also elevate your ankle at a level above your heart for 48 hours to help reduce swelling.
The recovery time is shorter for ankle sprains that do not require surgery. Grade One sprains may heal in about six weeks. Grade Two and Three Sprains may take several months to heal. Grade Three Sprains usually involve a period of physical therapy to promote healing.
Surgery
Ankle Sprains rarely require surgery; however, it is an option when non-surgical treatments and rehabilitation fail. Your physician will evaluate each case of Ankle Sprain on an individual basis. Your physician will discuss surgical options and help you determine the most appropriate choice for you.
In some cases of chronic pain, an Arthroscopic Surgery may be performed to remove bone fragments, scar tissue, and damaged cartilage. Arthroscopic surgery uses a small camera, called an arthroscope, to guide the surgery. Only small incisions need to be made and the joint does not have to be opened up fully. This can shorten the recovery time.
Recovery
Depending on the grade of the injury and what surgical or non-surgical methods are applied to repair the ankle, will determine the rate of recovery.
Recovery from surgery differs and depends on the extent of your injury and the type of surgery that was performed. Your physician will let you know what to expect. Individuals usually wear a cast for up to 2 months following surgery. Your doctor will instruct you to carefully increase the amount of weight that you put on your foot. Rehabilitation following surgery is a slow process. Individuals typically participate in physical therapy for two to three months. Physical therapy helps to strengthen the ankle muscles and increase movement. Success rates are high for both surgical procedures. The majority of individuals achieve an excellent recovery in about six months.
Prevention
Individuals that experience one ankle sprain are at an increased risk to experience another. It may be helpful to wear shoes that provide extra ankle support and stability. Shoes with low heels and flared heels may feel steadier. In some cases, doctors recommend a heel wedge or prescribe an orthosis, a plastic brace, to help position the foot inside of the shoe.
Low Back Pain
Introduction
Low back pain is very common. Muscle, ligament, nerve, and spine injuries are frequent causes of low back pain. Poor posture during movements and “wear and tear” can also cause low back pain. Degenerative diseases, such as arthritis, can cause the spinal structures to break down and put pressure on the spinal cord or nerves. Nerve pressure in the lumbar spine can cause symptoms to spread to the buttocks, legs, and feet. This is because the nerves that exit the spinal cord at the lumbar spine travel to these areas.
A medical examination is necessary to identify the cause of low back pain in order to determine the appropriate course of treatment. The majority of people with low back pain find relief with non-surgical treatments. However, for a small number of people with low back pain, symptoms progress or persist, and surgery can be an effective treatment.
Causes
Low back pain is caused by abnormalities in the soft tissues, nerves, discs, or vertebrae of the lumbar spine. The soft tissues--muscles, tendons, and ligaments, can strain from over exertion, poor posture, lifting activities, physical stress, and injury. Soft tissue injuries can cause painful muscle spasms or tightening of the lower back muscles.
Compressed, pinched, or irritated spinal nerves can cause symptoms that extend from the low back, through the buttocks and legs, and down to the feet. This commonly occurs from structural changes in the spine. Bone spurs, abnormal bone overgrowths caused by Osteoarthritis, can grow in to the spinal canal or nerve root openings on the vertebrae. Bone spurs and some degenerative diseases can also contribute to a condition in which the spinal canal is narrowed, called Spinal Stenosis. Some degenerative diseases cause the spinal structures to thicken and extend into the spinal canal over time. The narrowed canal causes pressure on the spinal cord and nerves.
Symptoms
The type of symptoms that you experience depends on the cause of your low back pain. Your pain may spread to your buttocks, legs, and feet. Your back may feel stiff, and you may not be able to completely move it. Your hips, legs, and feet may feel weak. You may also have numbness or tingling in your legs, feet, or toes. If you experience a loss of bowel or bladder control, you should seek medical attention immediately. A list of common causes of spinal related lower back pain and a description of symptoms is listed below.
Pressure on the spinal cord or spinal nerves can cause symptoms that radiate to your feet. Symptoms of Sciatica include shooting pain, tingling, weakness, and numbness that may travel from the lower back, through the back of one leg, and into your foot. You may feel burning pain, tingling, weakness, or numbness in your calf, foot, or toes. The weakness may be so bad that you cannot move your foot, bend or extend your knee, or walk. You may have difficulty moving from a seated position to standing up because of shooting pain. Additionally, your pain may become worse when you sneeze, laugh, cough, bend backwards, or have a bowel movement.
Diagnosis
Your doctor can determine the cause of your low back pain. The cause must be identified in order to treat your symptoms appropriately. Your doctor will perform a physical examination. Your doctor will ask you about your symptoms and medical history. You will be asked to perform simple back and leg movements to help your doctor assess your muscle strength, joint motion, and joint stability. Your doctor will test the reflexes and sensation in your legs. Your doctor may order lab studies to rule out diseases or conditions that can cause low back pain but are unrelated to the spine.
Your doctor may also order Computed Tomography (CT) scans, a Discogram, or Magnetic Resonance Imaging (MRI) scans to get a better view of your spinal structures. CT scans provide a view in layers, like the slices that make up a loaf of bread. The CT scan shows the shape and size of your spinal canal and the structures in and around it. A CT scan is useful for determining which disc is damaged. Your doctor may inject dye into the disc area to enhance the CT images in a procedure called a Discogram. A Discogram provides a view of the internal structure of a disc and can help to identify if it is a source of pain. The MRI scan is very sensitive. It provides the most detailed images of the discs, ligaments, spinal cord, nerve roots, or tumors. X-rays, myelograms, bone scans, CT scans, and MRI scans are painless procedures and simply require that you remain motionless while a camera takes the pictures.
Treatment
The treatment for low back pain depends on its cause, severity, and duration. The majority of low back symptoms are treatable with pain medications, short periods of rest, and exercise.
You may wear a back belt at the onset of pain for support. Over-the-counter medication or prescription medication may be used to reduce your pain. If your symptoms do not improve significantly, your doctor may inject your back with pain relieving medication.
Physical therapists can provide treatments to reduce you pain, and muscle spasms. They will show you exercises to gently stretch and strengthen your back and abdominal muscles. Your therapists will also show you proper postures or body mechanics to use during movements, such as how to position your back when lifting. The use of proper body mechanics can help to prevent further injury.
Surgery
Non-surgical treatments for low back pain are designed to relieve pain and restore function, but they can not correct structural deformities, such as narrowing of the spinal canal. Surgery is recommended when non-surgical methods have provided minimal or no improvement of your symptoms. Surgery may be required if a herniated disc, bone spur, or narrowed spinal canal is pressing directly on a nerve or the spinal cord. Surgery may also be required to stabilize a fractured vertebra after a traumatic injury. The goals of lumbar spine surgery are to remove the pressure from the nerves or spinal cord and establish spinal stability. There are several options for surgery, depending on the cause of the low back pain. Some of the more common surgeries are described below.
A Laminectomy is the most common surgery for Spinal Stenosis. This surgery is also used for relieving the symptoms of Sciatica caused by a disc herniation. The goal of a Laminectomy is to relieve the pressure on the spinal cord and nerves by enlarging the spinal canal where it has narrowed. To do so, the surgeon removes all or part of the lamina on the affected vertebrae. If all of the lamina is removed, the procedure is called a Laminectomy. A Laminotomy involves removing only part of the lamina.
A Discectomy is a type of surgery used to remove the part of a disc or fragments of bone that are putting pressure on the spinal cord or nerves. Commonly, this is performed through a small incision and with the use of a microscope. This is called a microdiscectony. In some cases, a Discectomy is performed in combination with a Spinal Fusion.
Spinal Fusion is the type of surgery most frequently used for Degenerative Disc Disease. Spinal Fusion involves fusing or securing the vertebrae together after removing the degenerative or herniated disc. The purpose of Spinal Fusion is to stop motion between spine segments, and relieve pain caused by this movement.
Recovery
Recovery from surgery depends on the cause of your low back pain and the type of surgery that you received. Most surgeries require at least an overnight stay in the hospital. Your doctor will let you know what to expect. You may need the help of a second person during the first few days or weeks when you return home. If you do not have a friend or family member nearby, talk to your doctor about alternative arrangements. Your doctor will also let you know when it is okay for you to drive again.
Prevention
It is important that you adhere to your restrictions and exercise program when you return home. It is important to keep your muscles strong and flexible. You should use proper body mechanics when lifting, sitting, and moving your body.
It can be helpful to maintain a healthy weight. Do not smoke. Smoking increases the risk of surgical complications and hinders bone fusing. Do not drive until your doctor has given you permission to do so.
4. Knee Arthroscopy
Introduction
The knee is the largest joint in our body. It is one of the most easily injured joints. Our knees are exposed and vulnerable to sport or work injuries. Knee problems can also occur from disease, aging, or “wear and tear.” Arthroscopic Knee Surgery, also called Arthroscopy, is the most accurate procedure to both diagnose and treat knee conditions.
Arthroscopy allows surgeons to see, diagnose, and treat problems inside the knee joint. Before arthroscopic surgery existed, surgeons made large incisions that affected the surrounding joint structures and tissues. They had to open the knee joint to see it and perform surgery. An arthroscopy requires small incisions and is guided by a small viewing instrument or "scope.” Arthroscopy is less invasive than traditional surgical methods. It has a decreased risk of infection and a shorter recovery period

Causes
Knee problems can occur from injury, disease, aging, or “wear and tear.” Any of the knee ligaments may be torn by an injury, especially during sports. The Medial Collateral Ligament most frequently tears during football, basketball, and volleyball. The Anterior and Posterior Cruciate Ligaments are frequently injured during football.
Overuse and “wear and tear” can cause the ligaments and synovium to become inflamed. They may swell and feel painful. Inflammation of the synovial membrane can occur with rheumatoid or gouty arthritis, as can bone deterioration. The knee bones can be fractured or broken during an injury. The patella may come out of its normal alignment and become unstable. The patella is commonly fractured from falls directly onto the knee.
Symptoms
Swelling and continuous pain are hallmark symptoms of knee injuries. Your knee may feel like it has a catch in it when you move it. It may suddenly give way as you stand or walk, causing you to fall.
Diagnosis
A doctor can evaluate your knee by gathering your medical history, performing a physical examination, and viewing medical images. Your doctor will ask you about your symptoms and what happened if you were injured. Your doctor will examine your knee and your leg alignment. You will be asked to perform simple movements to help your doctor assess your muscle strength, joint motion, and stability.
Your physician will order X-rays to see the condition of the bones in your knee and to identify arthritis. Sometimes a fracture or soft tissue injury does not show up on an X-ray. In this case, your doctor may order a Magnetic Resonance Imaging (MRI) scan. A MRI scan will provide a very detailed view of your knee structure. Like the X-ray, the MRI does not hurt and you need to remain very still while the images are taken.
Treatment
Most knee conditions can be treated with non-surgical methods. This includes medication, knee bracing, and physical rehabilitation. Arthroscopy is recommended when such treatments have provided minimal or no improvement of your symptoms. Arthroscopy is commonly used to reconstruct ligaments and remove or repair torn meniscal cartilage, synovium, or bone fragments. Your doctor will discuss your examination results and help you decide on your course of treatment.
Surgery
Almost all arthroscopic knee surgeries are performed as outpatient procedures. You will be asked to complete a physical examination prior to your surgery. You may be sedated for the surgery or receive a local or regional anesthetic. Local anesthesia will numb your knee area, and regional anesthesia will numb you below the waist. General anesthesia may also be used.
Recovery
After surgery, you will be instructed to elevate your leg and apply ice to your joint to help reduce pain and swelling. Your surgeon may restrict your activity and may recommend that you wear a knee brace for a short period of time following your procedure. You will need to use crutches, a walker, or a cane to help you walk at first.
Your doctor may set temporary or permanent physical restrictions for you depending on your type of injury. Your injury itself may restrict you form performing certain activities. For instance, if part of your menisci needed to be removed, you may be restricted from performing running activities or lifting large amounts of weight.
Prevention
Once you have injured your knee, it is important to avoid another knee injury. Talk to your surgeon about your activity precautions. It can be helpful to exercise to keep the muscles around your knee joint strong.
5. Humerus Fracture - Broken Upper Arm
Introduction
Humerus fractures are common. The humerus is the long bone in your upper arm. A fracture is a broken bone. The humerus is most frequently fractured as the result of a fall or motor vehicle crash. Depending on the location and severity of the fracture, some bones may heal without surgery. Fractures that are very unstable are realigned and held in place with surgical hardware. Physical rehabilitation usually follows either form of treatment and is an important part of recovery to regain use of the shoulder and upper arm.

Causes
Trauma is the main cause of humerus fractures. Most injuries result from a direct impact to the body, such as during a fall or motor vehicle crash. Older adults may experience humerus fractures from relatively minor falls.
There are different types of humerus fractures. They are named for the area of the bone that is broken. Proximal humerus fractures occur near the shoulder. Mid-shaft fractures are located in the middle of the bone. Distal humerus fractures are located near the elbow joint and are more common in children than in adults.
Symptoms
Humerus fractures cause severe pain and swelling. It may be very difficult for you to move your upper arm. If the nerves are affected, you may experience unusual sensations in the hand and weakness in your hand and wrist.
Diagnosis
Your doctor can diagnose a fractured humerus by examining your arm and taking X-rays. In rare cases, more sophisticated imagery, such as a computed tomography scan is used to provide a more detailed view.
Treatment
If the fractured bones are still in their proper position, a sling can be used to support and keep the arm from moving while it heals. Most mid-shaft humerus fractures can heal with immobilization and usually do not require surgery. Casting is not commonly used.
Your doctor will determine when you can begin physical therapy. Your therapists will help you move your shoulder joint at first with passive range of motion exercises. These exercises help improve circulation and reduce stiffness. You will proceed to more advanced exercises to increase strength and motion.
Surgery
If the fractured bones have moved out of position, surgery is recommended. Surgery called an Open Reduction and Internal Fixation (ORIF) is used to realign the bones and secure them in position with surgical hardware, such as plates, pins, screws, and wires. Surgery is most frequently used for proximal and distal humerus fractures.
For severe proximal humerus fractures, a shoulder replacement surgery is used to remove the damaged bone and insert an artificial implant. Severe proximal humerus fractures may also require reattachment of the shoulder muscles (rotator cuff muscles). Rehabilitation therapy, as described above, begins as soon as possible.
Recovery
The recovery process is different for everyone, depending on the severity of the injury and the treatment you received. Most fractures heal in about 4 to 6 weeks, but severe injuries may take longer to heal. Your doctor will let you know what to expect.
6. Hip Fracture - ORIF
Introduction
Hip Fractures are most commonly caused by falls. The risk for Hip Fractures increases with age. Older adults, especially those over the age of 85, are at the highest risk because of changes in bone structure and overall health. Medical complications from hip fractures can be life threatening. Because of the possible serious consequences, you should see your doctor or go to the Emergency Department of a hospital immediately if you suspect that you fractured your hip.

Causes
A Hip Fracture is caused by trauma. A Hip Fracture occurs when the top part of the Femur breaks. Falls are the most common cause of Hip Fractures in older adults, and the risk increases with age. Automobile crashes, a source of high force trauma, can cause Hip Fractures at any age.
Women experience more Hip Fractures than men. Women may be more susceptible because of differences in their skeletal structure and bone composition. Additionally, women may have higher rates of bone density loss from Osteoporosis, a bone weakening disease. For both women and men, bone density generally decreases after the age of 50.
Symptoms
You will feel pain when your Femur breaks. The pain will increase when you attempt to move your thigh. You may not be able to stand or put weight on your leg. Your leg may turn outward at an extreme angle or appear to be shorter than your other leg. If you suspect that you fractured your hip, you need to be seen by your doctor or go to the Emergency Department of a hospital immediately.
Diagnosis
Your doctor will make a diagnosis by examining you and asking you what has happened to cause the injury. Doctors order X-rays to confirm a Hip Fracture. X-rays provide a good picture of the bones in the hip joint. They can show exactly where the Femur broke and how far out of place the pieces have moved.
Some fractures do not show up on X-rays. Your doctor might order a Magnetic Resonance Imaging (MRI) scan for a very detailed view of your hip structure. Like the X-ray, the MRI scan is painless and requires you to remain very still while the images are taken.
Treatment
Treatment for Hip Fractures typically involves surgery. The rare exception is for individuals that cannot tolerate the risks associated with anesthesia. In a very small number of cases, the fracture is allowed to heal while the individual remains in bed for several weeks. This is very risky with respect to the development of other significant medical problems.
Surgery
Hip Fracture surgery is highly individualized. The type of surgery depends on the location of the fracture. Your surgery can take place as soon as you are medically stable. This is an in-patient surgery, requiring hospitalization. You will be admitted to the hospital for the surgery and can expect to spend a few days there while you recover.
You will have spinal or general anesthesia for the surgery. Your surgeon will make an incision at your hip and realign your broken bones. This procedure is called an Open Reduction. Your surgeon will use surgical hardware, termed Internal Fixators, to hold your bones in place while they heal. The complete surgical procedure is called an Open Reduction and Internal Fixation (ORIF).
Recovery
The recovery process from hip surgery is very individualized. Your doctor will tell you what you may expect. Generally, it takes about six to eight weeks for a hip fracture to heal. However, full recovery takes much longer.
You will need to use a walker or crutches while standing and walking. Your doctor will let you know how much weight to put on your foot. Your doctor will use an X-ray to see how your bones have healed.
Prevention
There are several ways that you can reduce the risk of falls and help to prevent a hip fracture. A general physical exam, bone density test, and an eye exam could identify medical conditions that are associated with dizziness or loss of balance. You should talk to your doctor or pharmacist about possible side effects or interactions associated with your medications. If you are susceptible to falls and live alone, it may be wise to wear a medical alert device to call for emergency help if needed.
7. Herniated Disc - Pain Management
Introduction
A herniated disc, also called a “ruptured” disc, is a common source of neck or lower back pain. Discs are cushion-like pads that are located between the series of small bones that make up the spine. A herniated disc occurs when the outer disc layer tears and it’s gel-like interior comes out. The contents can irritate nerves. A herniated disc can cause pressure on the nerves or spinal cord. Fortunately, for the vast majority of people, pain related to a herniated disc can be relieved without surgery.
Causes
With age, the discs lose water content. The discs become narrower, less flexible, and less effective as cushions between the vertebrae. As a disc deteriorates, the annulus fibrosis (outer layer) can tear or rupture. A herniated disc results when the nucleus pulposus (inner contents) come out of the disc.
In addition to the natural aging process, herniated discs can result after sudden pressure. Impacts from trauma, violence, and motor-vehicle crashes can cause a herniated disc. Abrupt forces during sports, such as football or surfing, can cause a herniated disc, as well.
Symptoms
The type of symptoms that you experience depends on the location of the herniated disc in your spine. Herniated discs most frequently occur in the cervical (neck) and lumbar (lower back) spine. Pain is a major symptom of a herniated disc, regardless of its location.
Neck pain is a common symptom of a herniated cervical disc. You may feel shooting pain in your arms. You may experience pain or burning pain in your shoulders, neck, and arms. Your arm(s) may feel weak, numb, or have a tingling sensation. You may experience a headache at the back part of your head.
In rare cases, the loss of bowel and bladder control along with significant arm and leg weakness indicates a serious problem. In this rare case, you should seek emergency medical attention. Call 911 or go to the nearest emergency department of a hospital.
Diagnosis
Your doctor can diagnose a degenerative disc by performing a physical examination and some tests. You will be asked about your symptoms and medical history. Muscle strength, joint motion, and stability will be tested. Because the nerves from the spine travel to the body, your doctor will perform a neurological examination of your arms and legs to see how the nerves are functioning.
An electromyography (EMG) test is often performed at the same time as the NCV test. An EMG measures the nerve impulses within a muscle. Healthy muscles need nerve impulses to perform movements. Your doctor will place fine needles into the select muscles that a spinal nerve controls. The EMG allows your doctor to determine the amount of nerve impulses that are conducted when your muscle contracts. An EMG may be uncomfortable, and your muscles may remain a bit sore following the test.
Treatment
The vast majority of people with herniated discs are successfully treated with non-surgical pain management treatments aimed at relieving pain and restoring function. Over-the-counter medication or prescription medication may be used to ease your pain. If your symptoms do not improve significantly with these medications, your doctor may inject your spine with corticosteroid medication to relieve pain at the source of the problem.
A short period of rest may be recommended. Your doctor may initially restrict your activity level and body positioning. You should avoid lifting, bending forwards, and quick abrupt movements. You may wear a back or neck brace for support. It can help to take brief walks and avoid sitting for prolonged periods.
Am I at Risk
Herniated discs are more common among people that are middle-aged. Older adults are at the greatest risk for herniated discs because of the decreased disc water content.
- Risk factors for herniated disc include:
- Being overweight
- Smoking
- Using poor body posture when lifting
- Performing repetitive strenuous activities
8. Heel Pain
Introduction
Your heels bear tons of pressure each day when you stand and walk. It’s no wonder that heel pain is a common complaint. Heel pain occurs for a variety of reasons, from wearing the wrong type of shoes to abnormal growths or tendon problems. Fortunately, most cases of heel pain can be treated without surgery. Talk to you doctor if you have heel pain. Early diagnosis and treatment can help prevent bigger problems.

Causes
Heel pain occurs for various reasons. Common causes of pain beneath the heel include bruising from stepping on something hard, inflamed connective tissue from overuse (plantar fasciitis), and irritated nerves under the heel. Rubbing from poorly fitted shoes, inflamed connective tissue (bursitis), or an inflamed tendon (Achilles tendon) most frequently cause pain behind the heel.
Symptoms
Symptoms of heel pain vary depending on the cause. It may develop gradually or occur suddenly. It may be accompanied by redness, thickened skin, or swelling.
Diagnosis
Your doctor will review your medical history and examine your heel to determine the cause of your pain. X-rays will be taken to check for bone abnormalities.
Treatment
Treatment for heel pain depends on several factors, including the cause and extent of the underlying condition. In many cases, rest, physical therapy, pain relievers, injections, proper shoes, and sole inserts can relieve symptoms. When such treatments fail, surgery may be recommended.
Surgery
Surgery may be used to relieve pressure from a nerve, remove an abnormal bone growth, or treat an inflamed tendon. Most surgeries for heel pain are performed as outpatient procedures. Following surgery, you will most likely participate in physical therapy to regain strength and motion.
Recovery
Recovery is an individualized process and depends on your condition and the treatment you received. Your doctor may recommend that you wear customized shoe inserts or orthopedic shoes. Your doctor will let you know what to expect.
9. Gout
Introduction
Gout is a disorder that can cause sudden joint pain. It occurs most commonly in the big toe, although it may affect other joints. The buildup of uric acid, a substance found naturally in the body and in certain foods, causes gout. Episodes of gout tend to come and go. Symptoms are treated with medications to ease pain and decrease inflammation. Measures can be taken to help prevent gout in some cases.
Causes
Gout is a type of arthritis that is caused by an excess of uric acid in the body. The surplus of uric acid causes needle-shaped urate crystals to form in the joints or surrounding tissues. The urate crystals cause pain and inflammation.
Symptoms
Gout usually begins with sudden symptoms, frequently during the night. Gout most commonly develops in the big toe, but it can also occur in almost any joint. Gout causes significant pain and tenderness. The joint may appear red and swollen.
Diagnosis
You should contact a doctor, such as a podiatrist, if you suspect that you have gout in your foot. Diagnosis and treatment are necessary to prevent joint damage. A doctor can diagnose gout by examining your joint and conducting some tests.
A joint fluid test is used to determine if urate crystals are in your joint fluid. Your doctor will use a needle to draw fluid from your joint for testing. Blood tests are used to test for the amount of uric acid in your blood. Your doctor will interpret the results of these tests to confirm a diagnosis of gout.
Treatment
Gout is treated with medications to relieve pain and inflammation, such as non-steroidal anti-inflammatory drugs, colchicine, and steroids. Your doctor may prescribe medications to decrease uric acid production in your body or to help your body remove uric acid. It may be helpful to limit foods that contain purines, such as red meat, and avoid drinking alcohol. It may be helpful to drink plenty of water to help the kidneys eliminate uric acid.
Surgery
You may help prevent gout by avoiding alcohol.
Avoid eating foods that are high in purines and limit the amount of protein from meat that you eat to about 5 or 6 ounces per day.
Am I at Risk
Gout most frequently develops in men between the ages of 40 and 50 years. Women who develop gout tend to do so after menopause when their levels of uric acid rise. Gout can be hereditary; meaning, if other people in your family have gout, your risk for the condition is increased.
- Risk factors for gout include:
- Consuming alcohol
- High blood pressure
- High cholesterol and high triglycerides
- Diabetes
- Arteriosclerosis- Narrowing of the arteries
- Low-dose aspirin
- Certain diuretic medications (thiazide diuretics) and anti-rejection medications for organ transplant recipients
Complications
In addition to causing gout, a build-up of uric acid can cause kidney stones. Untreated gout can lead to advanced gout, which is associated with nodules of urate crystals that form under the skin (tophi). For some people, gout is a recurring condition that happens several times a year.
10. Tendon Injuries (Hand)
Introduction
A flexor tendon injury occurs when the tendon is cut or ruptures. The flexor tendons attached at the palm side of your fingers and thumbs. They allow your finger and thumb joints to bend, grasp items, and perform fine coordinated movements. The muscles that control these tendons are in the forearm. Lacerations, other trauma, and rheumatoid arthritis are the primary causes of flexor tendon injuries.
Flexor tendon injuries can cause loss of movement, pain, and swelling. Flexor tendon injuries require surgical repair. Splinting and hand therapy rehabilitation usually follow surgical treatment.
Causes
Deep cuts are the main cause of flexor tendon injuries. They may also occur during sports, such as football, wrestling, rugby, and rock climbing. Rheumatoid arthritis can cause flexor tendons to rupture. The outward injury often appears simple, but is usually complex when involving the tendons and possibly the nerves.
Symptoms
A flexor tendon injury can cause your finger joints to feel painful and swollen. It may be difficult or impossible for you to move your finger. You may not be able to bend your finger joints. Nerves are located very close to the flexor tendon. If the nerves are injured, your finger may feel numb.
Diagnosis
Your doctor can diagnose a flexor tendon injury by reviewing your medical history and examining your wrist, hand and fingers. You should tell your doctor if you sustained an injury. Your doctor will carefully move your finger joints. Your doctor will test the sensation and blood flow to your fingers. X-rays can identify bone injuries.
Treatment
Flexor tendon injuries do not heal well without surgical repair. When a flexor tendon separates, the two pieces pull away from each other, making it impossible for the tendon to heal without surgery.
Surgery
There are many ways to surgically repair flexor tendons. Certain types of injuries need specific types of surgery. Your hand surgeon will stitch the ends of the tendon together and repair damaged nerves, blood vessels, or bones. A splint will immobilize your hand to allow the flexor tendon to heal after surgery.
Recovery
Hand therapy rehabilitation and continued splinting follow flexor tendon repair surgery. Hand therapy will help you regain strength, flexibility, motion, and functional use of your hand. Recovery from flexor tendon surgery is very individualized and rarely is full normal motion regained. Therapy protocols vary and will depend on the nature of your injury and repair. Splint protection is generally required for six weeks. Healing continues for three months after repair. Your doctor will let you know what to expect.
11. Broken Thigh Bone
Introduction
The bone in your thigh is called the femur. It is the strongest bone in the body. The femur is very difficult to break or fracture, but it can, as the result of a high impact vehicle crash or fall from a great height. Treatment for a femur fracture depends on the location and type of break in the bone, as well as the age of the person.
Anatomy
The femur is the long bone in your thigh. The long part of the bone is called the shaft. The top of the femur (femoral head) is part of the hip joint. The lower part of the femur helps form the knee joint.
Causes
Femur fractures result from high impact forces, such as those experienced in a high-speed vehicle collision or fall from a height. Older adults may experience femur fractures near the hip or the knee side of the bone after a fall, as the result of osteoporosis, a degenerative bone disease.
Symptoms
Femur fractures can cause severe pain, swelling, and bruising. Your leg may look shorter or out of its normal position. You may not be able to move your leg.
Diagnosis
Your doctor can diagnose a femur fracture by examining your leg and taking some X-rays. X-rays of the pelvis and knee joints may be taken as well. Your doctor will evaluate the nerves and blood vessels in your limb.
Treatment
Casting may be used to treat young children with a fracture in the shaft of the femur. A spica cast is used to immobilize the hips and the other leg.
Surgery
Most femur fractures are treated with a surgical procedure called intramedullary fixation. The procedure entails inserting a rod (intramedullary nail) into the center of the bone. The rod is secured with surgical screws. The rod provides support and stability while the fracture heals. After the fracture has healed, the hardware serves no further purpose, and may be removed.
Recovery
Physical therapy rehabilitation usually follows treatment. You will learn exercises to increase range of motion, flexibility, and strength. People that receive intramedullary fixation may be able to bear weight and walk sooner than people may with other types of treatments.
12. Diabetic Foot
Introduction
Foot problems are a common complication of Diabetes. Diabetes is a disease that affects how the body uses glucose, a sugar that is a source of fuel for the body. Normally, insulin, a hormone, helps glucose get into the body cells so that it is used for energy. People with diabetes either do not produce enough insulin or the insulin does not work like it should. Therefore, glucose does not get into the body cells. As a result, there is too much sugar in the blood, which can make people ill and result in medical complications. Diabetes is manageable. People with diabetes need to be aware of the possible associated medical problems.
Diabetes-related foot problems are most frequently caused by nerve damage and poor blood circulation. Infections, ulcers or sores, deformities, and trauma can all be the result. Foot problems are the leading reason for diabetes-related hospitalization. Further, diabetes is the leading cause of lower leg and foot amputation. Technology, research, and most importantly, diligence by individuals with diabetes can greatly improve the management of diabetes and reduce the risk of foot complications.
Causes
The feet are very vulnerable to diabetes-related complications. Further, there are a variety of foot problems that can occur. Diabetes-related foot conditions are most frequently caused by poor blood circulation, infection, and nerve damage that can result in ulcers or sores, deformities, and trauma.
Diabetes can often lead to nerve damage called peripheral neuropathy. Peripheral neuropathy is a condition in which nerve function deteriorates in the limbs. This leads to a gradual loss of feeling in the hands, arms, legs, and feet. This is often problematic because pain is what enables you to know when something is wrong. Without pain, you may not realize that you have bruises, cuts, blisters or burns and seek medical treatment. It is important that people with diabetes receive medical treatment for foot sores because diabetes-related circulation problems can lead to more problems.
Charcot foot is another common foot deformity associated with diabetic neurogenic arthropathy. Neurogenic arthropathy is a progressive degenerative arthritis that results from nerve damage. Charcot foot most frequently affects the metatarsal and tarsal bones located in the midfoot and forefoot.
Diagnosis
Your doctor can diagnose diabetic foot problems with a physical examination. Your doctor will ask you about your symptoms. There are a variety of tests your doctor may use to diagnose a problem with your foot. Testing is individualized depending on your symptoms and examination findings. Some of the most common assessments are described below.
Non-invasive vascular tests can provide information about the blood circulation in your feet. Your doctor can measure the amount of oxygen in your blood with a transcutaneous oxygen measurement. Your doctor will simply place sticky patches on your skin for this assessment. The blood pressure in your arm and ankle can be compared using the ankle-brachial index (ABI).
Your doctor may order an angiography to see the condition of the blood vessels in the legs and feet. An angiogram is a type of X-ray for the blood vessels. You will receive a small harmless injection of a radioactive substance that will highlight the blood vessels on the X-ray image.
A bone scan is useful for identifying bone abnormalities that are often associated with diabetes. A bone scan may show fractures, tumors, infection, and bone deterioration. A bone scan requires that you receive a small harmless injection of a radioactive substance. The substance collects in areas where the bone is breaking down or repairing. Further, three-phase bone scans and radiolabeled leukocyte scans are tests for determining the presence of infection.
Treatment
Overall, people with diabetes must monitor their blood glucose levels carefully, eat a balanced diet, exercise regularly, and see a physician routinely to prevent and stay on top of any problems that might develop. There are several options for diabetes-related foot problems. Treatment is individualized. It will depend on the source and severity of your foot problem. Your doctor will discuss appropriate treatment options with you.
Non-surgical treatments for diabetes-related foot problems include splinting, casting, or bracing to correct bone deformities. Your doctor can recommend proper footwear to provide structure and improve blood circulation. This may include a custom-walking boot. Your doctor can also provide medications or treatments for infections and skin ulcers.
Surgery
The main goal of treatment is to improve the integrity of the foot and reduce the risk of surgery and amputation. Surgery is considered for deformities that are too severe for a brace or shoe. Surgery may also be required to resolve advanced skin ulcers. In extreme cases, surgical amputation of the toes, foot, or leg is required to prevent further health problems and protect the remaining limb.
Recovery
Recovery from diabetes-related foot problems is different for everyone. It depends on the type of problem you experienced and the type of treatment you received. Because diabetes-related foot problems can be progressive, it is extremely important that you reduce your risk of complications and amputation by following preventive measures.
Prevention
- The following are tips to help prevent diabetes-related foot problems:
- Monitor your blood glucose levels carefully, eat a balanced diet, and exercise regularly. See a physician regularly to prevent and stay on top of any problems that might develop.
- Inspect your feet daily. Examine your feet for redness, warmth, blisters, ulcers, scratches, cuts, and nail problems. Feel for hard or dry skin. Look at the bottoms of your feet and between your toes. Use a mirror or have someone else look for you to check the bottom of your feet for redness or cracking.
- Examine the inside of your shoes for foreign objects, protruding nails, and rough spots before putting them on.
- Have custom-molded orthotics or shoes made by a foot specialist. The special footwear can help prevent ulcerations and infections in the feet.
- Buy shoes late in the day and never buy shoes that need "breaking in." Shoes should be comfortable the minute you put them on. Select shoes with deep toe boxes and made of leather upper material. Do not wear new shoes for more than two hours at a time and do not wear the same shoes every day.
- Contact your foot doctor immediately if you experience ANY injury to your foot or if you notice any changes in your feet. Even a minor injury is important for a person with diabetes.
- Do not file down, shave or remove calluses or corns yourself. This should ONLY be done by a foot specialist.
- DO NOT SMOKE! It decreases the blood supply to your feet. • Ask your doctor about precautions for soaking your feet.
- Do not trim your own toenails. Your foot specialist should do this.
- Do not use any strong antiseptic solutions on your feet. Iodine, salicylic acid, and corn or callus removers can be dangerous.
- Do not wear socks or stockings with tight elastic backs and never use garters.
- Do not wear any socks with holes and always wear shoes with socks.
- You should never use any type of sticky product such as tape or corn plasters on your feet. They can tear your skin.
- In the winter, wear warm socks and protective footwear. Avoid getting your feet wet in the snow and rain and avoid letting your toes get cold.
- Keep feet away from heat--hot water bottles, heating blankets, radiators, and heating pads. Burns can occur without your knowledge. Water temperature should always be less than 92 degrees. Estimate the water temperature with your elbow or bath thermometer.
- Lubricate your entire foot if your skin is dry but avoid putting cream between your toes.
- NEVER walk barefoot.
13. deQuervain's Tendonitis - Wrist Tendonitis
Introduction
De Quervain’s Tendonitis is a condition caused by an inflammation of the tendons located at the thumb side of the wrist. Tendons are tissues that attach our muscles to our bones. They can become swollen and sore from over use. Traditionally, de Quervain’s Tendonitis was called “Washer Woman’s Syndrome.” This is because the repetitive hand movements used for wringing wet clothes-- thumb pinching, squeezing, and moving the wrist outwards towards the little finger, are the motions that can cause de Quervain’s Tendonitis.

Causes
Doctors do not know what causes de Quervain’s Tendonitis. It may be produced by an irritation of the tendons at the base of the thumb.
Repetitive thumb motions and wrist deviation, moving the wrist towards the side, can irritate the tendons when they move through the tendon sheath. Activities that require such motions include wringing laundry, gardening, and the awkward hand movements required for lifting and caring for a new infant.
Overuse can cause the tendons to swell and accumulate fluid, resulting in a condition called Tendonitis. The lining of the tendon sheath can also become inflamed. This condition is called Tenosynovitis. Tendonitis and Tenosynovitis can occur independently or at the same time.
Tissue swelling associated with metabolic disorders, such as diabetes and rheumatoid arthritis, may also cause de Quervain’s Tendonitis. It appears to have a tendency to develop during pregnancy or menopause, times when fluid may be retained. Doctors also believe that de Quervain’s Tendonitis may be caused by direct trauma to the wrist or by a sudden strain from lifting or unaccustomed exercise.
Symptoms
The main symptom of de Quervain’s Tendonitis is pain at the thumb side of the wrist. You may also feel pain in your forearm. The pain can occur suddenly or gradually. The pain will usually become worse when you use your thumb and wrist to perform grasping and pinching motions. If the nerve that lies on top of the tendon sheath is irritated, it can cause the back of your thumb and index finger to feel numb.
De Quervain’s Tendonitis can also cause swelling at the wrist and thumb area. Some individuals develop a fluid-filled cyst in this region. You may hear crackling noises or feel a catch when you move your thumb. Some people have difficulty moving their thumb and wrist.
Diagnosis
Your doctor can diagnose de Quervain’s Tendonitis by examining your wrist and hand. Your doctor will also ask you about your symptoms and activities. The Finkelstein test is a common physical examination used to confirm a suspected case of de Quervain’s Tendonitis. The test is simple to perform. Your doctor will ask you to make a fist with your thumb tucked inside. Next, you will bend your wrist towards the little finger side of your hand. The test is positive if you feel pain at the base of your thumb.
Treatment
For some people, refraining from the activities that cause discomfort will make the symptoms go away on their own. Some cases of de Quervain’s Tendonitis respond to treatments that relieve pain and provide rest. Your doctor may recommend that you wear a splint to support and rest your joints. Anti-inflammatory medication may help reduce your pain and swelling. Sometimes doctors choose to inject cortisone into the tendon sheath.
Surgery
Surgery is recommended when symptoms persist and do not improve. The surgery is usually an outpatient procedure. You may be sedated for the surgery or the area will be numbed with regional or local anesthesia. Your surgeon will make an opening in your wrist and make an incision in the sheath that covers the tendon. Your surgeon may also remove the swollen tissue in the sheath. This creates a larger space for the inflamed and swollen tendons to move in. Occasionally, an occupational therapist can help you gradually gain strength and movement while reducing discomfort and swelling.
Recovery
Recovery from de Quervain’s Tendonitis is very individualized. It depends on the type of treatment used and the extent of surgery. Your doctor will be able to tell you what to expect. Most individuals have very good results and make a full recovery.
14. Clavicle Fracture - Broken Collar Bone
Introduction
Clavicle fractures are a common orthopedic injury, especially among infants and young children. The clavicle, known as the collarbone, is a long bone located at the top of the chest. A clavicle fracture most frequently results from trauma. The majority of clavicle fractures can heal without surgery. If surgery is necessary, the bone is secured with surgical hardware, such as plates and screws.
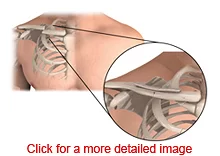
Anatomy
The clavicle is a long bone located on the upper chest. It is part of the shoulder joint. The clavicle provides stability for arm movements. The clavicle is not fully developed (ossified) until the late teens or early 20s.
Causes
Trauma is the main cause of clavicle fracture. A forceful impact to the shoulder area during a motor vehicle collision, a fall, or sports can break the clavicle. Newborns can experience a fractured clavicle as the result of a difficult birth.
Symptoms
You may hear a snapping sound and feel immediate pain when the clavicle breaks. The pain may increase and become sharp with movement. Bruising and swelling are common. If the bone has moved out of position, it may appear as a bump under the skin. Your shoulder area may not look as upright as usual. It may appear slumped forward and downward.
Diagnosis
You should contact your doctor immediately or go to the emergency department if you suspect you have broken your clavicle. Your doctor will review your medical history and conduct a physical examination. X-rays are taken to see the location and extent of the fracture.
Treatment
Clavicle fractures are most commonly treated with slings or a figure eight splint. A sling supports the arm and positions the shoulder to allow the fracture to heal. A figure eight splint wraps around the front of the shoulders and crosses in the back. It helps to maintain shoulder posture while the bone heals. Over-the-counter or prescription medications are used for pain relief. You may participate in rehabilitation therapy to help regain strength and motion following splinting or surgery.
Surgery
The majority of clavicle fractures can be treated without surgery. However, opinions about surgery are ever changing. Recent research shows that many patients that were not treated with surgery have had persistent problems. Your doctor will discuss the benefits of both procedures .
Recovery
Recovery from clavicle fracture is individualized and somewhat influenced by the age of the person. Children may heal in three weeks, and adults may take four to six weeks to heal. People can generally return to their full activity level in about 12 weeks.
15. Carpal Tunnel Syndrome (CTS)
Introduction
Carpal Tunnel Syndrome is a common condition that affects the hand and wrist. It occurs when the Median Nerve in the wrist is compressed. Nerves carry messages between our brains, spinal cord, and body parts. The Median Nerve carries signals for sensation and muscle movement. When the Median Nerve is compressed or entrapped, it cannot function properly. This syndrome has received much attention in the last few years because of suggestions that it may be linked with jobs that require repeated use of the hands. In actual fact, little proof of this exists.
Carpal Tunnel Syndrome is more common in women and people between the ages of 30 and 60 years old. It is the most common nerve entrapment syndrome and affects up to 10% of the population. Individuals with Carpal Tunnel Syndrome may feel numbness, pain, and a “tingly” sensation in their fingers, wrists, and arms. They may have difficulty performing grasping and gripping activities because of discomfort or weakness.

Causes
Carpal Tunnel Syndrome develops when the tissues and tendons in the Carpal Tunnel swell and make the area within the tunnel smaller. This can happen in association with other medical conditions, such as hypothyroidism and diabetes. The increased pressure within the tunnel causes the Median Nerve to become compressed. The pressure disrupts the way the nerve works and causes the symptoms of Carpal Tunnel Syndrome. Usually, the exact cause of carpal tunnel syndrome is unknown.
Rheumatoid arthritis, joint dislocation, and fractures can cause the space in the tunnel to narrow. Some women develop Carpal Tunnel Syndrome because of swelling from fluid retention caused by hormonal changes. This may occur during pregnancy, premenstrual syndrome, or menopause.
Symptoms
The primary symptoms of Carpal Tunnel Syndrome are pain, numbness, and tingling. The numbness and tingling is typically present in the thumb, index, middle, and half of the ring finger. Some people describe the pain as a deep ache or burning. Your pain may radiate into your arms. Your thumb may feel weak and clumsy. You may have difficulty grasping items, and you may drop things. Your symptoms may be more pronounced at night, when you perform certain activities, or in cold temperatures.
Diagnosis
Your doctor can diagnose Carpal Tunnel Syndrome by conducting a medical examination, reviewing your medical history, and asking you about your activities and symptoms. During the physical exam, your doctor will check your wrist and hand for sensation and perform a thorough hand examination.
Your doctor may ask you to perform a couple of simple tests to determine if there is pressure on the Median Nerve. For the Phalen’s Test, you will firmly flex your wrist for 60 seconds. The test is positive if you feel numbness, tingling, or weakness. To test for the Tinel’s Sign, your doctor will tap on the Median Nerve at the wrist. The test is positive if you feel tingling or numbness in the distribution of the median nerve. Lab tests may be ordered if your doctor suspects a medical condition that is associated with Carpal Tunnel Syndrome. Your doctor may take an X-ray to identify arthritis or fractures.
Treatment
The symptoms of Carpal Tunnel Syndrome can often be relieved without surgery. Some medical conditions associated with Carpal Tunnel Syndrome can be treated. Some cases respond to treatments that relieve pain and provide rest. Your doctor may recommend that you wear a splint at night to support your wrist in a neutral position.
Surgery
Surgery is recommended when non-surgical options do not work or if the condition becomes worse. There are a few types of outpatient surgery to remove pressure on the Median Nerve. Your doctor will help you decide which option is best for you.
The standard surgery for Carpal Tunnel Syndrome is called an Open Release.. Endoscopic Carpal Tunnel Release most often uses a local or regional anesthetic to numb the wrist and hand area. In some cases, individuals are sedated for the surgery. The surgeon makes a small opening below the crease of the wrist and inserts the endoscope to view the Carpal Tunnel. Some surgeons make a second incision in the palm of the hand. Guided by the endoscope, the surgeon places a tube called a cannula along the side of the Median Nerve. A special surgical instrument is inserted through the cannula that makes an incision in the Transverse Carpal Ligament. This surgery also opens the Carpal Tunnel and makes it larger to take pressure off of the Median Nerve. Because Endoscopic Carpal Tunnel Release spares some of the tissue in the palm, individuals may heal faster and experience less discomfort.
Recovery
Following surgery, your incision will be wrapped in a soft dressing. Your physician may recommend that you wear a splint to provide support and promote healing. You will be able to move your fingers immediately after surgery. You will need to avoid heavy grasping or pinching motions for about six weeks. Your doctor may recommend that you participate in occupational or physical therapy to gain strength, joint stability, and coordination. It may take several months for strength in the wrist and hand to return to normal.
Prevention
There are several things that you can do that may help prevent the symptoms of Carpal Tunnel Syndrome. A general physical examination could identify medical conditions that are associated with Carpal Tunnel Syndrome. An early diagnosis may allow for optimal treatment.
16. Neck Pain
Introduction
The neck is a very vulnerable part of the spine. It is susceptible to injury. Muscle, ligament, nerve, and spine injuries are common causes of neck pain. Poor posture and “wear and tear” can also cause neck pain. Degenerative diseases, such as arthritis, can cause the spinal structures to break down and put pressure on the spinal cord or nerves.
Neck pain can spread to the head, shoulders, arms, and hands. It can be acute or chronic. Acute neck pain begins suddenly, usually after an injury. Acute neck pain resolves as the injury heals, usually within several days or weeks. Chronic neck pain lasts longer than three months. Chronic pain may be constant and caused by structural changes in the spine from degenerative diseases.
A medical examination is necessary to identify the cause of the neck pain and to determine the appropriate course of treatment. Neck pain is usually treated with non-surgical methods. However, if symptoms progress or continue, there are a variety of spinal surgeries to relieve neck pain.
Causes
Neck pain is caused by abnormalities in the soft tissues, nerves, discs, or vertebrae of the neck. The soft tissues--muscles, tendons, and ligaments, can strain from over exertion, poor posture, physical stress, and injury. Motor vehicle crashes, sports, falls, or violence are causes of neck injuries. Soft tissue injuries can cause painful muscle spasms or tightening of the neck muscles.
The spinal cord or spinal nerves cause neck pain when they are compressed, pinched, or irritated. This commonly occurs from structural changes in the spine. Bone spurs, abnormal bone overgrowths caused by Osteoarthritis, can grow in to the spinal canal or nerve root openings on the vertebrae. Bone spurs can also contribute to a condition in which the spinal canal is narrowed, called Spinal Stenosis. Some degenerative diseases can cause the spinal structures to thicken and extend into the spinal canal over time. The narrowed canal causes pressure on the spinal cord and nerves, resulting in pain.
Symptoms
The type of pain that you feel depends on the cause of your neck pain. Your pain may range from mild to severe. The pain may begin suddenly and gradually get better, or it may start gradually and persist over time. The pain may spread to your head, shoulders, arms, and hands. You may get headaches. Your neck may feel stiff. You may not be able to completely move your neck. Your shoulder, arm, and hand muscles may feel weak. You may also experience numbness or tingling in your forearm, hand, or fingers.
You should seek immediate medical attention if you experience severe neck pain following an injury, such as from a motor vehicle crash, diving accident, or fall. You should not move your neck until it can be examined. To avoid the risk of further injury or paralysis, a medical professional should immobilize your neck. In rare cases, the loss of bowel and bladder control accompanied by significant arm and leg weakness indicates a serious problem. If you experience these symptoms, you should also seek immediate medical attention.
Diagnosis
Your doctor can determine the cause of your neck pain. The cause must be identified in order to treat your symptoms appropriately. Your doctor will perform a physical examination. Your doctor will ask you about your symptoms and medical history. You will be asked to perform simple neck movements to help your doctor assess your muscle strength, joint motion, and joint stability. Your doctor will test the reflexes and sensation in your arms and legs. Your doctor may order lab studies to rule out disease processes that may affect your neck.
A bone scan may be used to show fractures, tumors, infections, or arthritis. A bone scan requires that you receive a small harmless injection of a radioactive substance several hours before your test. The substance collects in your bones in areas where the vertebrae are breaking down or repairing. Your doctor may also order Computed Tomography (CT) scans, a Discogram, or Magnetic Resonance Imaging (MRI) scans to get a better view of your spinal structures. CT scans provide a view in layers, like the slices that make up a loaf of bread. The CT scan shows the shape and size of your spinal canal and the structures in and around it. Your doctor may inject dye into the disc area to enhance the CT images in a procedure called a Discogram. A Discogram provides a view of the internal structure of a disc and can help to identify if it is a source of pain. The MRI scan is very sensitive. It provides the most detailed images of the discs, ligaments, spinal cord, nerve roots, or tumors. X-rays, myelograms, bone scans, CT scans, and MRI scans are painless procedures and simply require that you remain motionless while a camera takes the pictures.
Treatment
The treatment for neck pain depends on its cause, severity, and duration. The majority of neck problems are treatable with pain medications, short periods of rest, and physical therapy. You may wear a soft neck collar for support.
Over-the-counter medication or prescription medication may be used to reduce your pain. If your symptoms do not improve significantly with these medications, your doctor may inject your neck with pain relieving medication. Occupational or physical therapists can provide treatments to reduce your pain, muscle spasms, and swelling. These include modalities, such as heat, ultrasound, and electrical stimulation. The therapists will also show you exercises to gently stretch and strengthen your neck muscles. Aquatic therapy may help ease your pain, relax your body, and provide support for you to exercise your joints.
Surgery
Surgery is recommended when non-surgical methods have provided minimal or no improvement of your symptoms. Surgery may be required if a herniated disc, bone spur, or a narrowed spinal canal is pressing directly on a nerve or the spinal cord. Surgery may also be required to stabilize a fractured vertebra after traumatic injury. The goals of neck surgery are to remove the pressure from the nerves or spinal cord and establish neck stability. There are several options for surgery, depending on the cause of the neck pain. Some of the more common surgeries are described below.
Recovery
Recovery from surgery depends on the cause of your neck pain and the type of surgery that was performed. Most surgeries require at least an overnight stay in the hospital. Your physician will let you know what to expect.
Individuals usually participate in physical therapy following surgery. Physical therapy exercises will help strengthen your neck muscles. Overall, most individuals achieve good results with surgery and are able to resume their regular lifestyles.
Prevention
It is important that you adhere to your restrictions and exercise program when you return home. It is important to keep your muscles strong and flexible. You should use proper posture when lifting, standing, sitting, and moving your body.
It can be helpful to maintain a healthy weight. Do not smoke. Smoking increases the risk of surgical complications and hinders bone fusing.
17. Neuropathy - Nerve Pain
Introduction
Neuropathy, also referred to as neuralgia or neuritis, is a type of pain that involves the nerves. Neuropathy results from nerve degeneration, pressure, inflammation, or infection. There are several causes of neuropathy, including carpal tunnel syndrome, pinched nerves, spinal stenosis, and pressure from spinal discs. Nerve pain management is individualized. Lifestyle changes including weight loss, regular exercise, and smoking cessation; and physical therapy can help relieve some types of pain. People with more significant symptoms may need medication or surgery to help relieve and manage pain.
Causes
Neuropathy is a type of pain that occurs when nerves in the peripheral or central nervous system are compressed, pinched, trapped, or affected by disease. Specific causes of neuropathy include:
- Nerve degeneration: Stroke, brain bleeding, multiple sclerosis
- Nerve pressure: Trapped nerve, pinched nerve
- Nerve inflammation: Ruptured disc, slipped disc
- Nerve infection: Shingles, viral infection
- Common types of neuropathy include:
- Entrapment Neuropathy
A trapped or pinched nerve at the neck, shoulder, elbow, wrist, hip, lower leg, or foot. Common examples of nerve entrapment include carpal tunnel syndrome, thoracic outlet syndrome (neck), or piriformis syndrome (hip). - Peripheral Neuropathy
Peripheral neuropathy first develops in the longest nerves of the body in a "glove and stocking" distribution to the hands and feet. There are numerous causes of peripheral neuropathy, including certain hereditary conditions, viral diseases, liver or kidney failure, and toxins, as well as diseases such as diabetes, vascular disease, and rheumatoid conditions. - Phantom Limb Pain
Phantom limb pain occurs in some people after the amputation of an arm or leg. Although the exact cause of phantom limb pain is unknown, it appears to result when the nerves and memories in the brain send faulty signals as the circuitry attempts to "rewire" itself. - Post Herpetic Neuralgia (PHN)
Post herpetic neuralgia (PHN) is a type of nerve pain that can occur following a viral infection of herpes zoster "shingles" in the nervous system. Post herpetic neuralgia aching or stabbing pain occurs in areas where the shingles rash developed. The skin in such areas may feel extra sensitive, especially in white-colored scars. - Post Traumatic Neuropathy
Post Traumatic Neuropathy occurs after injury or medical procedures, such as surgery or injection. Nerve pain symptoms may arise at the injury site and nerve path. - Trigeminal Neuralgia (TN)
Trigeminal neuralgia (TN) is a cause of severe pain in the face and jaw. Shocking, electric "lightening" pains typically precede dull aching pain. Trigeminal neuralgia usually affects only one side of the face. The exact cause of trigeminal neuralgia is unknown, but it develops where the trigeminal nerve is compressed, pinched, or irritated.
Symptoms
The nervous system itself does not have its own receptors or system for pain. Because it has no system for sending pain signals, the nerve sends faulty signals when it is injured. The brain misinterprets these signals as pain that feels sharp, shooting, burning, or hypersensitive. Other symptoms of nerve malfunction include tingling, numbness, intense itching, weakness, and hypersensitivity to cold, heat, or vibration.
Nerve pain can travel to locations where the nerve normally travels. For example, sciatica is a type of nerve pain that originates in the lower spine. Sciatica pain may travel down the sciatic nerve into a leg and foot.
Diagnosis
A doctor can diagnose neuropathy and the source of pain by reviewing your medical history, conducting a medical examination, and asking you about your activities and symptoms. Your doctor may ask you to perform certain tasks as part of a neurological exam. Your doctor may use lab tests, nerve studies, or diagnostic imaging tests determine what is causing pain, depending on the condition that you may have.
- Common studies to aid diagnosis include:
- Computed Tomography (CT) - Computed Tomography (CT) provide views in slices that a computer manipulates into 3D images of bones and dense tissues.
- Electromyography (EMG) - Electromyography (EMG) measures the nerve impulses in muscles to identify poor nerve input.
- Magnetic Resonance Imaging (MRI) - Magnetic Resonance Imaging takes very detailed images of internal body structures.
- Nerve Conduction Velocity (NCV) - Nerve Conduction Velocity (NCV) measures how well a nerve works and can help identify the site of compression.
- X-rays - X-rays use radiation energy to create images of internal body structures. X-rays do not provide as much detail as CT or MRI.
Treatment
Pain management for nerve pain is very individualized. The type of treatments and techniques pain management doctors prescribe depends on the cause, location, and extent of your nerve pain.
Stress and tension can increase pain. You can learn techniques to help you relax. Improving your lifestyle can help too. It is beneficial to get plenty of sleep, lose weight and maintain a healthy weight, and eat a well-balanced diet. You should avoid alcohol, cigarettes, and illegal drugs.
Weak muscles lead to more pain than healthy strong muscles do. It is helpful to perform regular stretching and strengthening exercises. Exercise can help relieve pain by stretching tight muscles and tissues. Physical therapists and occupational therapists can set up an exercise program just for you. Your therapists can also teach you how to use proper lifting techniques and postures to prevent injury.
Surgical methods may be appropriate after considering other pain relief treatments. There are several surgical methods for pain management. Spinal cord stimulation involves the surgical placement of a small device in the back or abdomen. The device transmits an electrical current to the spinal cord so that you feel a tingling sensation instead of pain. Small pain pumps can be surgically placed under the skin to deliver a continuous flow of pain relieving medication. Intradiscal electrothermal therapy (IDET) uses heat to treat injured discs and nerves. Percutaneous stereotactic rhizotomy uses heat to destroy the nerves that cause pain.
18. Osteoarthritis of the Knee
Introduction
Osteoarthritis is the most common type of arthritis, affecting more than 21 million Americans. Osteoarthritis tends to develop as people get older or from overuse of the knee during work or sports. Osteoarthritis causes the protective covering at the ends of the bones in the knee to gradually wear away, resulting in painful bone on bone rubbing and disrupted movement. Medications, physical therapy, and knee injections are used to treat osteoarthritis of the knee. Surgery may be necessary if pain and immobility limit your activities and lifestyle, despite non-surgical treatments.
Causes
Osteoarthritis of the knee occurs as the articular cartilage in the knee joint breaks down, causing a reaction in the bone. The bones in the knee joint become thicker and develop growths (osteophytes or spurs). Lubricating fluid in the joint (synovial fluid) gets thicker and inflamed. If too much fluid is produced, a condition referred to as "water on the knee" can result. With osteoarthritis, the knee joint continues to experience changes over several years. Eventually, very little of the articular cartilage remains. Bone-on-bone rubbing causes pain, impairs knee movements, and makes daily activities difficult.
- Factors that increase the risk of developing osteoarthritis include:
- Excess weight or obesity that adds pressure to the knee joints
- Heredity
- Increasing age
- Women more than 50 years old have a higher incidence than men
- Knee injury
- Repetitive stress injury to the knee
- Participation in high impact sports
- Certain illnesses, including septic arthritis and metabolic disorders
Symptoms
Osteoarthritis of the knee can cause knee pain and swelling. You may have difficulty moving your knee or performing activities such as walking, squatting, kneeling, and going up or down stairs.
Diagnosis
Doctors diagnose osteoarthritis of the knee by examining the knee, considering your symptoms, and reviewing your medical records. X-rays are the main diagnostic tool to diagnose osteoarthritis.
Treatment
Treatment of osteoarthritis of the knee is individualized. The treatment that you receive depends on several factors, including your overall health and the stage of disease. Osteoarthritis of the knee is treated with physical therapy, lifestyle changes, medications, surgery, or a combination of treatments.
If you are overweight , your doctor may recommend that you lose weight. Attaining and maintaining a healthy weight reduces the load on your knees. Participating in physical therapy can help strengthen the muscle groups around the knee joint. A knee brace can provide support.
Your doctor may recommend over-the-counter pain medications such as aspirin or nonsteroidal anti-inflammatory drugs. Your doctor may prescribe stronger prescription pain medications if necessary. Joint injections, such as corticosteroid injections or viscosupplementation, are used for osteoarthritis pain relief.
Surgery
If symptoms persist despite conservative treatments, knee surgery may be necessary. Osteotomy and joint replacement (arthroplasty) are surgical procedures to treat osteoarthritis of the knee. Osteotomy is used to remove and reshape bone from the leg to cause a shift in body weight away from the damaged area. Casting, splinting, and physical therapy follow osteotomy. Recovery from osteotomy varies from 3 to 6 months for some people, and up to a year for others.
19. Osteoporosis
Introduction
Osteoporosis is the most common bone disease. It causes progressive bone loss and increases the risk of fractures. Osteoporosis is more common in women than men, and the incidence increases with age. Bone loss from osteoporosis can lead to fractures and disability. The progression of osteoporosis may be reduced with treatments, including dietary changes, nutrition supplements, exercise, and medications.
Causes
Although the exact cause of osteoporosis is unknown, there are several factors that may contribute to the condition. As you grow older, new bone production decreases, resulting in a reduced total bone mass. People with small bones or a family history of fractures have a greater risk of developing osteoporosis. The risk for women increases at menopause when estrogen levels drop. Poor nutrition, a low calcium diet, smoking, excessive alcohol intake, and a lack of regular exercise are lifestyle factors that may contribute to osteoporosis. Medications, such as steroids or anticonvulsants, and some illnesses, such as thyroid disorders or bone cancer, can cause osteoporosis.
Symptoms
Osteoporosis does not cause symptoms in the early stages of the disease. As osteoporosis progresses, you may experience bone tenderness or pain, particularly in your neck or low back. You may develop stooped posture and a loss of height. For many, bone fractures are the first sign of osteoporosis. The spine, wrists, or hips are common fracture sites.
Diagnosis
Your primary care physician or gynecologist may assess you for osteoporosis. You should tell your doctor about your risk factors. Bone mineral density (BMD) testing is an evaluation used to help diagnose osteoporosis. It is a type of X-ray test called a dual-energy x-ray absorptiometry (DEXA). BMD testing is recommended for women under the age of 65 with risk factors other than menopause, postmenopausal women with fractures, and all women age 65 and older. Additional X-rays, computed tomography (CT) scans, blood tests, and urine tests may be used.
Treatment
Lost bone cannot be replaced, but further bone loss can be prevented. Treatments are also aimed at reducing pain and preventing fall-related fractures. Your doctor will make nutrition and exercise recommendations for you. Calcium and Vitamin D supplements are commonly advised. Weight bearing exercises, such as walking, can help prevent bone loss and possibly increase bone density. It is also helpful to reduce the risk factors that you can control, such as quitting smoking.
There are several different types of medications that are used to treat osteoporosis. Your doctor will review the risks and benefits of the medications with you. Bisphosphonates and hormone replacement therapy are used to treat osteoporosis in postmenopausal women. Newer anti-estrogen medications, such as Raloxifene, are selective estrogen receptor modulators (SERMs). SERMs act similar to estrogen to increase bone density, reduce the risk of fractures, and lower the risk of breast cancer. Calcitonin is a medication that eases pain and slows the bone loss process. Alendronate is a newer FDA approved medication to help prevent bone loss from osteoporosis.
Prevention
Osteoporosis cannot be cured, but its progression may be prevented with medication, diet, and exercise. You should reduce the risk factors that you can control, such as not smoking or drinking alcohol excessively.
Am I at Risk
- More women than men develop osteoporosis. The condition is more common in people that are Caucasian or Asian. Risk factors may increase your chance of developing osteoporosis. Risk factors include:
- Increasing age is a risk factor for osteoporosis. With aging, calcium and phosphate substances that make bones strong, are reabsorbed by the body causing bones to become weaker.
- Decreased estrogen levels in women after menopause increases the risk of osteoporosis.
- Lowered testosterone levels in men with aging increases the risk of osteoporosis.
- Excess corticosteroid production from Cushing’s syndrome, hyperthyroidism, and hyperparathyroidism increases the risk of osteoporosis.
- Bone cancer may cause osteoporosis.
- Immobility or being confined to a bed may increase the risk of developing osteoporosis.
- Osteopenia, abnormally low bone density, may lead to osteoporosis.
- People with a family history of osteoporosis have a greater risk of developing osteoporosis.
- Certain medications, such as steroids and anticonvulsants, can cause osteoporosis.
- Absent menstrual periods (amenorrhea) or early menopause may increase the risk of osteoporosis.
- Smoking and heavy alcohol consumption increases the risk of osteoporosis.
- Eating disorders and low body weight increase the risk of osteoporosis.
- A lack of calcium in your diet increases the risk of osteoporosis.
Complications
Bone loss from osteoporosis can lead to fractures, particularly in the spine, wrist, and hips. Hip fractures are a leading cause of admittance to nursing homes.
Advancements
Researchers are working on developing a urine test to diagnose early osteoporosis. This may expedite treatment and help to reduce the effects of osteoporosis.
20. Platelet-Rich Plasma (PRP) Therapy
Introduction
Platelet-Rich Plasma (PRP) Therapy is a cutting-edge procedure that is revolutionizing the field of orthopedic medicine. PRP therapy is a new treatment that relieves pain and promotes long lasting healing of musculoskeletal conditions. PRP Therapy uses components of the body’s own blood cells to formulate a customized “cocktail” that stimulates the natural healing process in certain orthopedic conditions.
The body’s first response to any soft tissue injury is to deliver platelet cells. Filled with healing and growth factors, platelets jump start the repair process and attract the essential aid of stem cells. PRP therapy’s natural healing process magnifies the body’s efforts by delivering a higher concentration of platelets through a simple injection.
PRP therapy is associated with reduction in pain and faster healing, and has lower risks and lower costs than surgery.
Causes
Platelet rich plasma (PRP) therapy is a rapidly emerging technique that is showing exciting potential, particularly with soft tissue injuries such as to tendons and ligaments.
A main benefit of PRP Therapy is that it provides pain relief and healing and can eliminate the need for surgery and prolonged recovery. It may also be used as a treatment for some people that are not candidates for surgery. PRP Therapy is a low-risk minimally invasive procedure. It uses the body’s own cells and natural biological healing process. The concentrated platelet rich plasma (PRP) that is injected into and around the point of injury jump-starts and significantly strengthens the body’s natural healing process. Recovery with PRP therapy is often much faster than with surgery. Because your own blood is used, there is no risk of a transmitting infection and a very low risk of allergic reaction.
Treatment
PRP Injections are a much simpler procedure than surgery. PRP Injections are short office procedures. To complete PRP therapy, a sample of your blood is drawn (similar to a lab test sample) and the blood is then spun at high speeds, separating the platelets from the other components. The concentrated platelet rich plasma (PRP) is then injected into and around the point of injury. No stitches are necessary since just a needle was used.
The procedure takes under an hour, including preparation and recovery time. Performed safely in the office, PRP therapy relieves pain without the risks of surgery, general anesthesia, or hospital stays and without a prolonged recovery. In fact, most people return to their jobs or usual activities right after the procedure.
Recent News
Recent news headlines have featured the amazing results that professional athletes have experienced with PRP Therapy. Pro football players Hines Ward and Troy Polamalu of the Pittsburgh Steelers received PRP Therapy after injuries that should have side-lined them for months, but they returned to play in a matter of weeks, winning the Super Bowl. Los Angeles Dodgers pitcher Takashi Saito received PRP Therapy for an elbow condition and returned to play in just a few months, versus up to 14 months that recovery from surgery would have taken. Unprecedented results have also been reported for other professional soccer, baseball, and football players. While PRP Therapy is just beginning to become mainstream news, it actually has been around for quite some time.
In the field of orthopedics, PRP Therapy is being studied for use in the joints, spine, bone, ligaments and tendons. Because the studies have used a small number of participants, larger studies are necessary before the results can be generalized. Researchers are optimistic that after future studies, insurance will cover the procedure, and speculate that the procedure may become a protocol before surgical treatment
21. Rotator Cuff Tear & Repair
Introduction
Rotator cuff tears are a common source of shoulder pain. The rotator cuff consists of four shoulder muscles and their tendons. Tendons are strong fibers that connect our muscles to our bones. The shoulder muscles and tendons cover the upper end of our arm bone forming a cuff.
The risk of rotator cuff tears increases with age. The aging process can cause the tendons and muscles to degenerate and weaken. Rotator cuff tears can also result from sudden shoulder movements or overuse, for instance during sports, such as pitching in baseball or playing tennis, or falls.
The decision on how to treat rotator cuff tears is very individualized. Some rotator cuff tears can be treated with non-surgical methods. However, surgical procedures have become less invasive, resulting in good outcomes with improved recovery times.
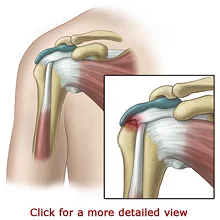
Causes
Rotator cuff tears most frequently occur in the dominant arm but commonly occur in the non-dominant arm. The risk of rotator cuff damage increases with age. With age, the blood supply to our tendons decreases. This causes the tendons and muscles to degenerate, weaken, and become susceptible to tearing. Additionally, the tendon degenerates with age. The body’s ability to repair the tendon decreases over time because of the reduced blood supply.
Sometimes the aging process can cause bone spurs to grow on the scapula, particularly in the acromion area. Shoulder impingement syndrome occurs when bone spurs or bursa inflammation narrows the space that is available for the rotator cuff tendons. The tendons can tear as they rub across the bone spur, particularly when the arm is elevated. Inflamed tendon membranes may develop tendonitis, a painful condition. Shoulder impingement syndrome may even cause the rotator cuff tendons to detach from the top of the humerus.
Rotator cuff injuries can occur in younger people following a shoulder injury, such as a fracture or dislocation. Overuse or repetitive activity can also cause rotator cuff tears. This includes athletes that perform overhead movements during such sports as tennis, swimming, or baseball. This also includes workers who reach upwards repetitively during construction, painting, or stocking shelves.
Symptoms
The symptoms of a rotator cuff tear tend to appear gradually. You may first develop pain in the front part of your shoulder. Your pain may spread down the side of your arm. The pain may be mild at first and increase when you lift your arm or lower your arm from a fully raised position. Over time, the pain may be present when you rest and even wake you while you sleep. However, some rotator cuff tears are not painful at all.
Your shoulder may feel stiff. It may be difficult for you to move your arm. You may hear a crackling noise when you do so. Your arm may feel weak, especially when your lift or rotate it.
The symptoms of a rotator cuff tear caused by traumatic injury occur suddenly. You may feel a snap and sudden pain. Your arm will immediately feel weak, and you will have difficulty moving it.
Diagnosis
A doctor can evaluate your shoulder by performing a physical examination and viewing medical images. Your doctor will ask you about your symptoms and medical history. You will be asked to perform simple movements to help your doctor assess your muscle strength, joint motion, and shoulder stability.
Your physician will order X-rays to see the condition of the bones in your shoulder and to identify arthritis or bone spurs. A special dye may be used with the X-ray in a procedure called an Arthrogram. Sometimes a soft tissue injury does not show up on an X-ray. In this case, your doctor may order a Magnetic Resonance Imaging (MRI) scan or an ultrasound. A MRI scan will provide a very detailed view of your shoulder structure. It will help your doctor determine the location and type of your rotator cuff tear. An ultrasound uses sound waves to create an image when a device is gently placed on your skin. These tests do not hurt but require that you remain very still while a camera takes images.
Treatment
Many rotator cuff tears can be treated with non-surgical methods including rest and pain relief. Limiting overhead arm movements and wearing a sling may help to reduce symptoms. Over-the-counter medication or prescription medication may be used to reduce pain and swelling. If your symptoms do not improve significantly with these medications, your doctor may inject your joint with corticosteroid medication. Corticosteroid medication is a relatively safe pain reliever. Physical and occupational therapy can be helpful to restore strength and function.
Surgery
Surgery is recommended when non-operative treatments have provided minimal or no improvement of your symptoms. Surgery may also be recommended for painful injuries or for people who rely on their arm strength for work or sports. There are several types of surgeries that can be performed for rotator cuff tears. The type of surgery that you have depends on the size, shape, and location of your tear.
Partial rotator cuff tears may only require debridement. This surgical procedure simply trims the tendon. Suturing the tendon together repairs a complete tear. Additionally, tendons can be reattached to the bone. Many of these surgeries can be done as outpatient procedures. You will be anesthetized for the surgery. Three common surgical approaches include Open Surgical Repair, Mini-Open Repair, and Arthroscopic Repair.
The arthroscope is used to remove bone spurs under the acromion and to treat other structures in the shoulder joint. Your surgeon will then use a mini-open incision to repair the rotator cuff. Results of the Mini-Open Repair are equal to the Open Repair surgical method.
Another option for rotator cuff repair is All-Arthroscopic Repair. This technique is commonly used to reconstruct ligaments or remove damaged tissue and bone spurs. Arthroscopy is less invasive than traditional surgical methods. It has a decreased risk of infection and a shorter recovery period.
Your surgeon will make one or more small incisions, about ¼” to ½” in length, near your shoulder joint. Your surgeon will fill the joint space with a sterile saline (salt-water) solution. Expansion of the space allows your surgeon to have a better view of your joint structures. Your surgeon will insert the arthroscope and may reposition it to see your joint from different angles.
Your surgeon may make additional small incisions and use other slender surgical instruments for surgical treatments. Because the surgical incisions are so small, they will require just a few stitches or Steri-Strips. Your surgeon will cover them with a bandage.
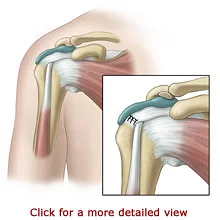
Recovery
Your shoulder will need several weeks to heal from the surgery. Your surgeon will restrict your arm movements for a short period of time following your procedure. You will most likely wear an arm sling for four to six weeks. An occupational or physical therapist will gently help you move your arm at first, and then you will progress to strengthening exercises.
Prevention
It may be helpful to exercise to maintain a strong, stable, and flexible shoulder. Avoiding repetitive overhead movements may help to prevent rotator cuff tears. Further, it is important to follow your doctor’s instructions for any weight lifting or motion restrictions.
22. Spondylolisthesis - Slipped Vertebrae
Introduction
Small bones, called vertebrae, align to form the spine in your back. A healthy spine supports the body, while allowing movement. Spondylolisthesis occurs when age or injury causes a vertebra in the lower back to slip forward and out of position.
Spondylolisthesis may not cause symptoms. Spondylolisthesis can cause back or leg pain. The majority of people with symptomatic spondylolisthesis are treated successfully with pain management and restoring function.
Causes
Spondylolisthesis results when a vertebra slips out of position in the spine. Degenerated facet joints or a fracture can cause a vertebra to move. With age, the facet joints can deteriorate, weaken and cause one vertebra to slip forward. This condition is called degenerative spondylolisthesis. A stress fracture in the pars on a vertebra (spondylolysis) can lead to isthmic spondylolisthesis, but this is rare occurrence. A vertebra that has moved out of position can press on nerves or narrow the size of the spinal canal (spinal stenosis).
Symptoms
Spondylolisthesis symptoms depend on how far the vertebra has moved out of position and if other structures or nerves are affected. In the vast majority of cases, spondylolisthesis does not cause symptoms. It can cause low back pain and stiffness. Muscle spasms can cause the hamstring muscles at the back of the thighs to tighten. The tightened hamstrings may feel stiff and can affect posture, making it difficult to walk.
Prolonged standing or walking may increase your symptoms. Bending forward or sitting may relieve symptoms because these positions increase the room in the spinal canal, taking pressure off the spinal cord.
If the spinal nerves in the lower end of the lumbar spine are compressed, a condition called Cauda Equina Syndrome may result. Cauda Equina Syndrome can cause loss of bladder and bowel control, as well as low back pain, leg pain, leg weakness, lower body sensory deficits, and reduced or absent leg reflexes. If you suspect you have Cauda Equina Syndrome, seek emergency medical treatment immediately.
Diagnosis
Your doctor can diagnose spondylolisthesis by reviewing your medical history and examining you. You should tell your doctor about your symptoms. You will be asked to perform simple movements to help your doctor evaluate your muscle strength, joint motion, and spine stability. X-rays are used to view the alignment of your spine. Additional imaging studies may be ordered to identify nerve root compression or spinal canal narrowing.
Treatment
Spondylolisthesis that does not cause symptoms does not need treatment. The majority of people with spondylolisthesis are treated without surgery. Treatments to relieve symptoms from Grade 1 and some cases of Grade 2 spondylolisthesis are aimed at pain management and improved function.
Pain relieving and anti-inflammatory medications may be used to ease symptoms. If your symptoms do not improve significantly with these medications, your doctor may recommend epidural steroid injections. Epidural steroid injections are used to place medicine directly near the source of pain and inflammation. Steroid medication is used to reduce inflammation and relieve pain. Epidural injections are short outpatient procedures that may be repeated over time.
Surgery may be needed for some people with a Grade 2 spondylolisthesis and those with Grade 3 or higher. Again, the overall percentage of people with spondylolisthesis that require surgery is relatively small. Surgery is necessary when the slipped vertebra is unstable, when symptoms are severe, and when nerve compression causes neurological symptoms. Spinal fusion surgery is used to secure the vertebrae together. A lumbar laminectomy surgery is used to enlarge the spinal canal to take pressure off the spinal cord or nerves.
Am I at Risk
- In rare cases, spondylolysis can precede spondylolisthesis.
- Degenerative spondylolisthesis occurs most frequently in people over the age of 65.
- Women experience spondylolisthesis more often than men do.
23. Sprains & Strains
Introduction
Sprains and strains are common injuries that can happen to anyone, but occur most frequently in people who participate in sports, perform repetitive activities, or are at-risk for falls. Sprains involve the tissues that connect bones together (ligaments). Strains involve a different group of tissues, muscles and the tendons that connect muscles to bones. Mild sprains and strains can heal with rest and home care. Significant sprains and strains may require rehabilitation, surgery, or both.
Causes
Sprain
A sprain describes an injury to a ligament that connects two bones. A ligament can stretch or tear if the bones in a joint move out of position from a force, such as a fall or direct contact with another person during sports. For example, an ankle or wrist sprain can result from a fall.
Strain
A strain describes an injury to a muscle or tendon. Muscles and tendons can be injured from overuse, overstretching, repetitive motions, sports injury, or a direct force, such as from being hit. For example, back strain may occur in people who perform repetitive heavy lifting.
Symptoms
Sprain
A sprain causes pain, bruising, and swelling. You may hear or feel a pop when the injury occurs. A severe sprain causes intense pain at the time of injury, followed by difficulty moving a joint.
Strain
A strain causes muscle pain, weakness, cramping, spasm, or swelling. Moderate to severe sprains can result in muscle tearing.
Diagnosis
A doctor can diagnose a sprain or strain by physical examination. Your doctor will ask you to move your joint and test your muscle strength. X-rays may be taken if a fracture is suspected.
Treatment
Immediately following your injury, you should elevate your joint and apply cold packs to prevent swelling. Your doctor will formulate a treatment plan based on the severity and degree of your injury. Mild sprains and strains may benefit from physical or occupational therapy following injury. More significant sprains and strains may require surgery or immobilization with a brace or splint for healing.
Am I at Risk
- Your body is deconditioned or overweight
- You participate in sports, dance, or other challenging physical activities
- Your job duties entail repetitive movements
- You have experienced a strain or sprain before
- You are at-risk for falls
Complications
Sprains and strains may be prevented by exercising and eating wisely to keep your body fit and healthy. You can help prevent sprains and strains by warming up and cooling down, respectively, before and after exercising. Be sure to wear the proper shoes and safety equipment for the sports or job duties in which you participate. Older adults should discuss fall-risk prevention with their doctors.
24. Tennis Elbow - Lateral Epicondylitis
Introduction
Tennis Elbow is a condition that results in deterioration of the tendon fibers that attach to the bone at the outside of the elbow. Tendons are strong fibers that attach muscles to bone. They are tissues that do not stretch easily and are susceptible to degeneration under repeated or traumatic stress. Another name for Tennis Elbow is Lateral Epicondylitis. The pain of Tennis Elbow occurs primarily where the tendons of the forearm muscles attach to the elbow bone at the Lateral Epicondyle. Playing racquet sports is only one cause of Tennis Elbow.

Causes
Tennis Elbow most commonly occurs in individuals between the ages of 30 and 50 years old. Tennis Elbow is caused by chronic stress to the forearm muscles, especially the Extensor Carpi Radialis Brevis. The repeated motions and stress can cause the tendon to degenerate (tendonopathy). As the name Tennis Elbow implies, playing tennis or other racquet sports is one cause of the condition; particularly, repeated use of the backhand stroke, forearm stroke, or serve with poor athletic form. Many individuals develop Tennis Elbow for no identifiable reason.
Symptoms
Individuals with Tennis Elbow frequently experience severe burning pain and tenderness at the outer side of their elbow and forearm. In most cases, the pain starts out slow and mild but gradually increases over weeks or months. The pain may increase with movement or when pressure is applied to the outer elbow area. Some individuals experience morning stiffness, muscle weakness, and aching throughout the day. They may be unable to perform the motions necessary to complete various tasks. Some individuals may even feel pain when they are not moving their arm.
Diagnosis
A physician will perform an examination and review the individual’s medical and activity history to make a diagnosis of Tennis Elbow. The physician evaluates the forearm structures by using simple tests. The history and examination, supplemented with X-rays of the elbow are sufficient to make the diagnosis. X-rays may be used to assess if the elbow bone was injured and help rule out other possible causes of elbow pain, such as arthritis. When taking an x-ray, a camera focuses on the elbow area and a picture is taken. Magnetic Resonance Imaging (MRI) scans are rarely used to diagnose Tennis Elbow however MRI scans may be used to provide a very detailed view of the tendon injury. The MRI equipment takes images by focusing on the elbow area. Both imaging techniques are painless and require that the individual remain very still.
Treatment
Most cases of Tennis Elbow respond to non-surgical treatments. Treatment typically includes rest or activity restriction/alteration. Specific exercises, often under the guidance of a therapist, are often prescribed. Physicians may instruct the application of ice to the affected areas or recommend medication to relieve pain. Wrist splints and forearm bands can be used to relieve symptoms and promote healing.
Tennis Elbow may also be treated with corticosteroid medications. Corticosteroid medication is a relatively safe pain reliever and in the case of tennis elbow would be injected at the outside of the elbow. After the pain is relieved, physical or occupational therapy may be needed. The physical or occupational therapists focus on improving physical functioning for participation in activities. The therapies address muscle strength, flexibility, endurance, and coordination. This method is successful for many individuals with Tennis Elbow.
Surgery
The majority of individuals with Tennis Elbow do not require surgery. Surgery is considered if significant pain continues after at least six months of treatment. The surgery is performed as an outpatient procedure. The individual may remain alert with regional anesthesia or be sedated for the surgery. The surgeon makes a small opening at outside of the elbow bone and then removes any injured tissue and reattaches the tendon to the bone. Recently, an arthroscopic surgery method has been developed. Arthroscopic surgery uses a small camera, called an arthroscope, to guide the surgery. Only small incisions need to be made and the joint does not have to be opened up fully. This technique can provide a positive outcome and a shortened recovery time.
Recovery
With non-surgical treatments, symptoms of Tennis Elbow may be relieved as early as four to six weeks. However, many individuals have chronic symptoms for many months. Individuals requiring corticosteroid injections or surgery may take several months to recover, but typically can achieve good results. Tennis Elbow does not usually lead to severe problems if it is treated. If left untreated, it rarely leads to loss of motion and function.
25. Total Hip Replacement
Introduction
The hip is one of the most commonly replaced joints. The hip is a ball and socket joint. It allows us to move our legs and bend and straighten our body. Osteoarthritis, a type of arthritis, is the main reason for Hip Replacement Surgery. Other conditions, including trauma, may also cause the need for a hip replacement.
Arthritis is a progressive and degenerative disease that causes joint pain, stiffness, and swelling. It affects the cartilage in the hip joint. Cartilage is a very tough, shock absorbing material that covers the ends of many of our bones. The cartilage forms a smooth surface and allows the bones in our joints to glide easily during motion. Arthritis causes the cartilage to wear away. Loss of the protective cartilage can cause painful bone on bone rubbing.

Causes
Arthritis is a major cause of joint pain, stiffness, and swelling in the hip. Arthritis can occur for many reasons, including aging, “wear and tear,” injury, disease, and developmental abnormalities of the hip structure. There are over 100 different types of arthritis. Osteoarthritis, Post-Traumatic Arthritis, and Rheumatoid Arthritis are types of arthritis that most frequently develop in the hip.
Osteoarthritis is the most common type of arthritis which typically develops as people grow older. Osteoarthritis can result from overuse of the hip during sports or work. Post-Traumatic Arthritis can develop in individuals of all ages after a hip injury, such as a fracture of the hip socket.
Osteoarthritis causes the articular cartilage covering the end of the bones to gradually wear away, resulting in painful bone on bone rubbing. Abnormal bone growths, cysts or spurs, can grow in the hip joint. They add to the pain and swelling, while disrupting movement.
Symptoms
The main symptom of severe hip arthritis is dull and aching pain. You may feel pain in your hip, groin, thigh, buttock, and sometimes in the knee. The pain may occur while you are moving or resting. It may even keep you awake at night. Your hip may feel stiff. You may have difficulty moving or lifting your leg. Your hip pain may eventually limit your everyday activities, including walking, stair climbing, and bending. Medications and physical therapy may provide relief from the pain of severe hip arthritis.
Diagnosis
Your doctor can diagnose arthritis by conducting a physical examination. You will be asked about your medical history, symptoms, and level of pain. You may be asked to perform simple hip and leg movements to help your doctor assess your muscle strength, joint motion, and hip alignment. Blood tests and other laboratory tests may identify what type of arthritis you have.
Your doctor will order X-rays to see the condition of your bones and to identify areas of arthritis, bone cysts, or bone spurs. Sometimes the tissues that surround the hip joint or the condition of the bones do not show up on an X-ray. In this case, your doctor may order Magnetic Resonance Imaging (MRI) scans or a bone scan. A MRI is used to obtain more detailed images. A bone scan identifies the location of abnormal growths in a bone, such as arthritis. A bone scan requires that you receive a small harmless injection of a radioactive substance several hours before your test. The substance collects in your bones in areas where the bone is breaking down or repairing itself. X-rays, MRIs, and bone scans are painless tests. However, they require that you remain very still while a camera takes pictures.
Treatment
As your arthritis progresses and becomes more severe, medication, rest, and physical therapy may fail to relieve your symptoms. Your pain and immobility may cause you to limit your activities and lifestyle. Hip Arthroplasty is recommended when non-surgical treatments do not provide relief of your symptoms.
Surgery
Hip Arthroplasty involves removing your damaged joint and replacing it with an artificial one. This is an inpatient procedure. You will most likely be admitted to the hospital on the day of your Arthroplasty and stay there for a few days.
The most common types of anesthesia for the surgery are general anesthesia or spinal anesthesia. The general anesthesia will put you to sleep. The spinal anesthesia will numb your body from the waist down, while you remain awake, but sedated, so your memory is blurred. Your doctor will help you decide which anesthesia is best for you. You may also be required to donate your own blood for transfusion during the surgery. This is usually done several weeks before your operation.
Your surgeon will make an incision on the side of your hip to access your joint. Your hip joint will be opened to allow your surgeon to remove damaged bone, cartilage, or connective tissue. The femoral head and the cartilage or bone from the hip socket will be removed.
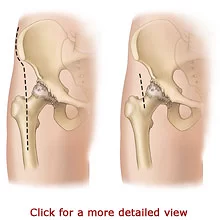
Recovery
You will stay in the hospital for two to five days following your Hip Arthroplasty and you will receive pain medication to make you as comfortable as possible. A V-shaped pillow may be placed between your legs to position your hip while it heals. You should sleep with a pillow between your legs for about six weeks. Your physician will temporarily restrict certain movements to prevent your artificial joint from dislocating. You should refrain from crossing your legs, bending your hips at more than a 90-degree angle, and pointing your feet inward or outwards depending on the surgical approach to your hip. It is important that you adhere to your exercise program and safety precautions when you return home. You may resume many of your former activities following your Hip Arthroplasty.
You may have to change the way you do some activities, such as bending, to protect your new hip. You will be advised to avoid high-impact sports, such as jogging, for the rest of your life. High-impact sports or weight gain can put stress on your artificial joint, causing it to become loose or wear faster. However, it is very important that you continue with your recommended exercise program.
It is important to avoid falling. Your therapists can suggest ways to prevent falls in your home. This may simply mean removing throw rugs and making sure that your walking path is free of cords and clutter. You should also continue to use the durable medical equipment as advised.
26. Total Knee Replacement
Introduction
The knee is the largest joint in our body. It is one to the most easily injured joints. Knee problems can occur from injury, aging, “wear and tear,” or disease, such as arthritis.
Arthritis causes joint pain, stiffness, and swelling. It can affect the cartilage in the knee joint. Cartilage is a very tough, shock absorbing material that covers the ends of many of our bones. The cartilage forms a smooth surface and allows the bones in our joints to glide easily during motion. Arthritis can cause the cartilage to wear away. Loss of the protective lining can cause painful bone on bone rubbing.
While the symptoms of knee arthritis may be tolerated with some medications and lifestyle adjustments, for many, knee replacement is the only way to reduce pain, restore function, and improve the quality of life. Knee Replacement Surgery, also called Knee Arthroplasty, involves removing the damaged portion of the knee and replacing it with artificial implants called prosthetics. Knee Arthroplasty is the most common type of joint replacement surgery. It is highly successful for relieving pain and restoring joint function.

Causes
Arthritis is the most common cause of knee pain, stiffness, and swelling. Arthritis can occur for many reasons, including aging, “wear and tear,” injury, disease, and developmental abnormalities in the knee structure. There are over 100 different types of arthritis. Osteoarthritis, Post-Traumatic Arthritis, and Rheumatoid Arthritis are types of arthritis that frequently develop in the knee.
Osteoarthritis is the most common type of arthritis. It tends to develop as people grow older. Osteoarthritis can result from overuse of the knee during sports or work. Osteoarthritis causes the articular cartilage covering the end of the bones to gradually wear away, resulting in painful bone on bone rubbing and disrupted movement.
Rheumatoid Arthritis is one of the most serious and disabling types of arthritis. Rheumatoid Arthritis can affect people of all ages, but most frequently occurs in women and those over the age of 30. It is a long-lasting autoimmune disease that causes the synovial membrane to become inflamed, which then attacks the cartilage. This damages the articular cartilage and leads to pain and stiffness.
Post-Traumatic Arthritis can develop in individuals of all ages after a serious knee injury. A knee fracture or severe torn ligaments can damage the cartilage over time. This can cause knee pain and limit function.
Symptoms
The main symptom of severe knee arthritis is moderate to severe pain. Your pain may occur while you are moving or resting. It may even keep you awake at night. Your knee may feel swollen, stiff, or unstable. It may look like it angles inward or outward, instead of being straight.
It may be difficult to move or bend your knee. Your knee pain may eventually limit your everyday activities, including walking, stair climbing, and getting in and out of chairs. Medications, rest, and physical therapy may provide little relief from the pain of severe knee arthritis.
Diagnosis
Your doctor can diagnose arthritis by conducting a physical examination. You will be asked about your medical history, symptoms, and level of pain. You may be asked to perform simple knee movements to help your doctor assess your muscle strength, joint motion, and knee alignment. Blood tests and other laboratory tests may identify what type of arthritis you have.
Your doctor will order X-rays to see the condition of your bones and to identify areas of arthritis. Your doctor may order Magnetic Resonance Imaging (MRI) scans or a bone scan. A MRI is used to obtain more detailed images of the ligaments and cartilage. A bone scan identifies the location of abnormal growths in a bone. A bone scan requires that you receive a small harmless injection of a radioactive substance several hours before your test. The substance collects in your bones in areas where the bone is breaking down or repairing itself. X-rays, MRIs, and bone scans are painless.
Treatment
As your arthritis progresses and becomes more severe, medications, rest, and physical therapy may fail to relieve your symptoms. Your pain and immobility may cause you to limit your activities and lifestyle. Knee Arthroplasty or replacement is recommended when non-surgical treatments do not provide relief of your symptoms.
Surgery
Knee Arthroplasty involves removing your damaged joint and replacing it with an artificial one. This is an inpatient procedure. You will most likely be admitted to the hospital on the day of your Arthroplasty and stay there for several days. In most cases, you will be required to donate your own blood prior to the surgery so you can be transfused during or after the procedure, if necessary.
Your knee will be placed in a bent position for your surgery. Your surgeon will make a six to twelve inch incision on the side of your patella (kneecap). Your patella and thigh muscles will be moved aside to allow your surgeon access to your joint. Your surgeon will remove your damaged bone, cartilage, and connective tissue. Your knee joint will be replaced with an artificial joint.
There are many types of artificial knee joints. Your surgeon will choose the most appropriate one for you, depending on your age, weight, activity level, and overall health. Nearly all of them consist of three components. The new piece for the end of your femur is made of highly polished metal. The tibial component, for the top of your leg, is made of metal and plastic. The patellar part is made of plastic and fits inside of your kneecap. The artificial pieces may or may not be cemented in place. The artificial joint will allow you to perform most of the pain-free movements that you used to be able to do.

Recovery
You may stay in the hospital for two or three days following your Knee Arthroplasty. You will receive pain medication to make you feel as comfortable as possible. Your doctor may use several methods to prevent blood clots and swelling.
Your doctor may prescribe blood thinning medication and special support stockings. You should keep your leg elevated and move or pump your foot and ankle. Your doctor may prescribe compression boots and a Continuous Passive Motion (CPM) Machine. Compression boots are inflatable leg coverings that are attached to a machine. They work to gently squeeze your legs to aid blood circulation. A Continuous Passive Motion (CPM) Machine will move your leg in a cycling motion while you are in bed. The CPM Machine is helpful to improve circulation, decrease swelling, and restore movement in your knee.
The success of your surgery will depend, in part on how well you follow your home care instructions during the first few weeks following surgery. You may need a little help from another person during the first few days at home. If you do not have family members or a friend nearby, talk to your physician about possible alternative arrangements. You should be able to resume most of your regular activities in three to six weeks after your procedure. Overall, the majority of people experience a dramatic reduction of knee pain and the ability to resume functional activities after Knee Arthroplasty.
Precautions
It is important that you adhere to your exercise program and safety precautions when you return home. You should stay as active as possible, but remember not to overdo it. You should notice a steady improvement in your strength and endurance over the next six to twelve months.
It is also important to avoid falling. Your therapists can suggest ways to prevent falls in your home. This may simply mean removing throw rugs and making sure that your walking path is free of cords or clutter. You should also continue to use the durable medical equipment as advised
